A study conducted in the University of Massachusetts found that there may be a possible genetic link between some mental health disorders such as schizophrenia and bipolar disorder, and type 2 diabetes.
The scientists found a gene DISC1, which is responsible for mental disorders such as bipolar disorder, schizophrenia, and some other forms of depression, triggers the release of pancreatic beta cells that store or produce insulin to normalize blood glucose level. Beta cells can recognize a spike in blood glucose level very quickly by secreting the stored insulin.
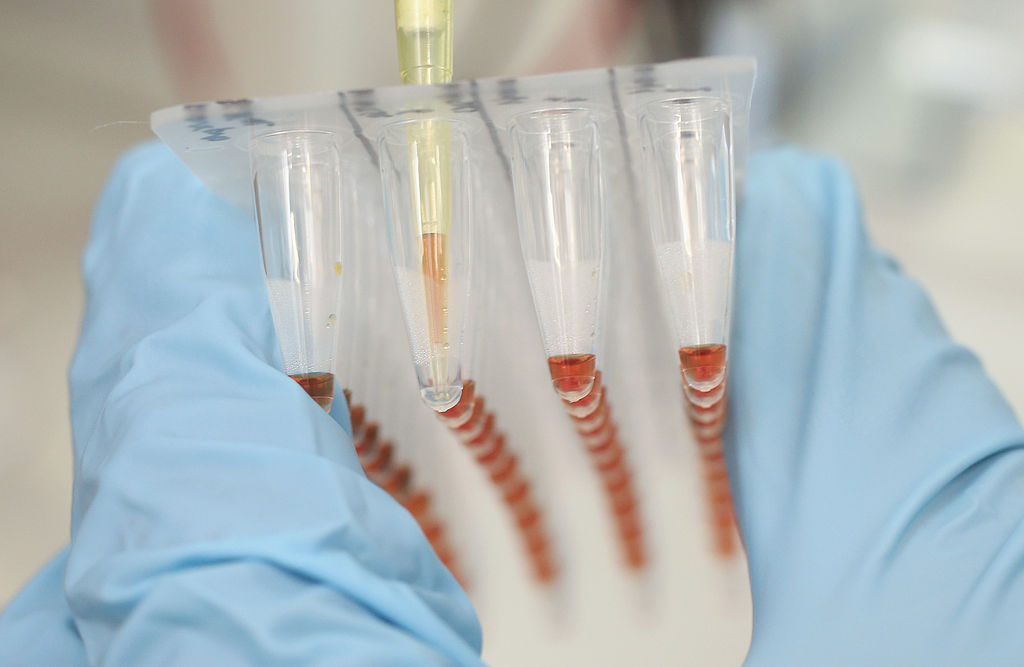
Rita Bortell, Ph.D. researcher in the Diabetes Center Of Excellence at the University of Massachusetts Medical School in Worcester, along with her colleagues studied the function of DISC1 on two groups of mice; one group with disrupted DISC1 gene (genetically manipulated) in the mouse's pancreatic beta cells and the second group of mice was normal.
The mice with disrupted DISC1 gene showed increased beta cell death leading to less insulin secretion and impaired glucose regulation while the mice in the control group were normal. DISC1 controls the activity GSK3B, a specific protein known to be critical for beta cell function and survival.
Researchers found that inhibition of GSK3B resulted in improved beta cell survival and restored normal glucose tolerance in mice with disrupted DISC1. Earlier studies had found connections between alterations in the DISC1 and increased risk of schizophrenia, but further studies have also found DISC1 alterations in individuals with bipolar disorder and major depression.
Bortell hopes that their finding linking disrupted DISC1 to diabetes and mental disorders may help to uncover mechanisms to improve therapies to reduce suffering caused due to illness that are extraordinarily costly and often debilitating, according to Science Daily.
The study was published in The FASEB Journal.
