Connective tissue cells in the heart turn into bone-producing cells in response to injury, University of California, Los Angeles scientists report November in Cell Stem Cell. The discovery helps explain why some people who survive heart damage develop abnormal calcium deposits--the main component of bone--in the valves or walls of the heart. The researchers also show that heart calcification can be prevented in mice by blocking an enzyme that regulates bone mineralization with small molecules.
Tissues outside of the bones don't naturally calcify, yet mineralization of organs, including the heart, blood vessels, and kidneys, occurs with age and is exacerbated in people with diabetes or kidney disease. In the heart, calcification can disrupt electrical conduction and lead to heart blocks. Once the calcium deposits form in tissues, there are currently no treatments to break them down.
"Heart calcification has been understudied and underreported," says senior author Arjun Deb, of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research based at the University of California, Los Angeles. "We asked the question, 'What are the cells in the heart that cause calcification?' and given the strong association between tissue injury, fibrosis, and calcification, we hypothesized that maybe it is cardiac fibroblasts [cells that give rise to scar tissue after injury] that are contributing to the calcification process."
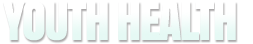
To find out, Deb and his co-authors genetically tagged cardiac fibroblasts in mice and watched as they transitioned into bone-forming, osteoblast-like cells after heart injury. The researchers transplanted the cardiac fibroblasts isolated from the region of calcification under the skin of healthy mice and observed soft-tissue calcification similar to that seen in the donor mice. Human cardiac fibroblasts were also observed to be capable of forming similar calcium deposits in a laboratory dish.
Deb and his team then asked whether heart calcification could be prevented or treated using small molecules. Their best lead for a drug target was a protein called ENPP1 that seemed to be overexpressed by the heart, and specifically by cardiac fibroblasts, in response to injury. The researchers injected several different small molecules that could disrupt the activity of ENPP1 and observed a decrease of 50% or more in the extent of calcium deposition. Injection of a drug called etidronate led to a 100% rescue with no calcification after injury.
"We now want to see whether this is a common pathway to calcification regardless of etiology and if what we found can be broadly applied to tissues across the body," says Deb, who also holds several posts at the UCLA David Geffen School of Medicine.
His research group has already begun looking in patient cells to see whether blood vessel calcification can be prevented using the small molecule approach. They also want to explore potential drugs that could render calcification reversible, as the ENPP1 approach only worked to prevent calcium deposits when injected in advance of injury.
Provided by CELL PRESS