The news out of the American Society for Clinical Oncology annual meeting seemed to be all about checkpoint inhibitor drugs that boost the immune system and a protein biomarker that may help determine which cancer patients will benefit from checkpoint inhibitors.
Checkpoint inhibitor drugs block a protein called PD-1 (which stands for programmed death receptor) that solid cancers use to hold the body's immune system at bay. These drugs include Keytruda and Opdivo, which have been found to be effective against some cancers, notably melanoma, but not as effective against others, such as lung cancer. Other checkpoint inhibitors are either on the market or in development.
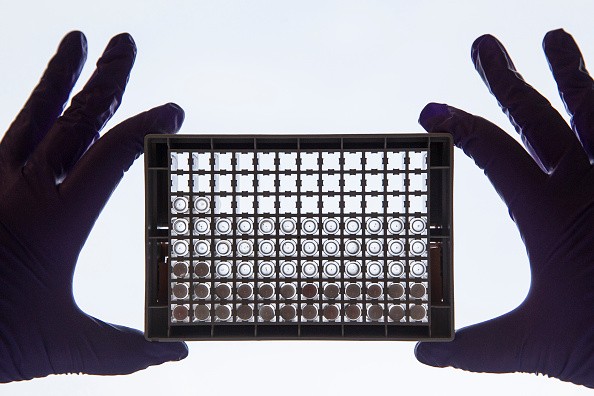
A study presented at the meeting found that Opdivo is most helpful in patients who have high levels of a related protein, PD-L1. This finding suggests that physicians should first take a biopsy from a tumor to test for PD-L1 to determine if Opdivo or other checkpoint inhibitors will work. Pharmaceutical firms are developing tests for these protein markers.
However, Reuters Health interviewed several researchers who believe that using protein levels this way may not be reliable. Tests for protein levels may vary depending on where in the tumor the biopsy is taken. They may also depend on how far the cancer has spread.
In addition, some patients who have tested negative for PD-L1 still benefited from treatment with Opdivo, which may mean that PD-L1 is the wrong biomarker.
Checkpoint inhibitors are very expensive drugs. Opdivo and Keytruda each cost about $12,500 per month. Because of these costs, health insurers want to find tests that will show which patients will benefit the most from the drugs and which will not benefit at all.
Drug companies are also starting to combine Opdivo and Keytruda with each other and with other treatments including older chemotherapy drugs and with experimental antibodies to PD-L1.



