The vaccine against human papillomavirus (HPV) appears to be more effective than previously thought. It has already reduced the prevalence in teen girls by 64 percent, according to a government report. HPV causes cervical and other types of cancer.
The percentage of girls and women who have received the HPV vaccine is still relatively low, but despite this, the effects are being seen. Even in women in their early 20s, who have lower vaccination rates than teens, several strains of human papillomavirus have been reduced by 34 percent.
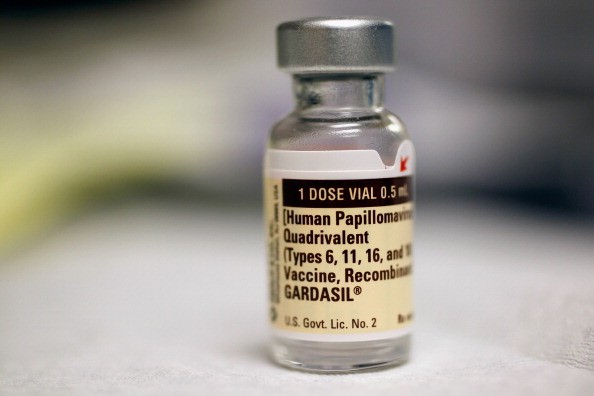
Even though the HPV vaccine has been shown to be effective, its use is still low. Only about 40 percent of girls and 20 percent of boys between the ages of 13 and 17 have been vaccinated. The vaccine has been controversial because HPV is sexually transmitted and therefore it is associated with adolescent sexual activity. Only three places-Virginia, Rhode Island and the District of Columbia-require that teens received the HPV vaccine.
The vaccine is recommended, but not required, for children ages 11 and 12, when the body has a stronger response and before sexual activity is begun. When the vaccinated person later has sex, they are protected against the strains of the virus that are most closely linked with cancer. Because they do not become infected, they are then less likely to spread the virus.
About 14 million Americans are infected with HPV each year, but most of them clear the virus from their bodies with no ill effects. But some strains persist and can cause genital warts, as well as cancer of the cervix, anus, penis, and mouth and throat. More than 4,000 women will die of cervical cancer each year, according to the American Cancer Society.
This research was published in the journal Pediatrics and is based on a survey by the U.S. Centers for Disease Control and Prevention. The study looked at HPV immunization and infection rates in girls through 2012 because the recommendation to vaccinate boys became widespread only in 2011.



